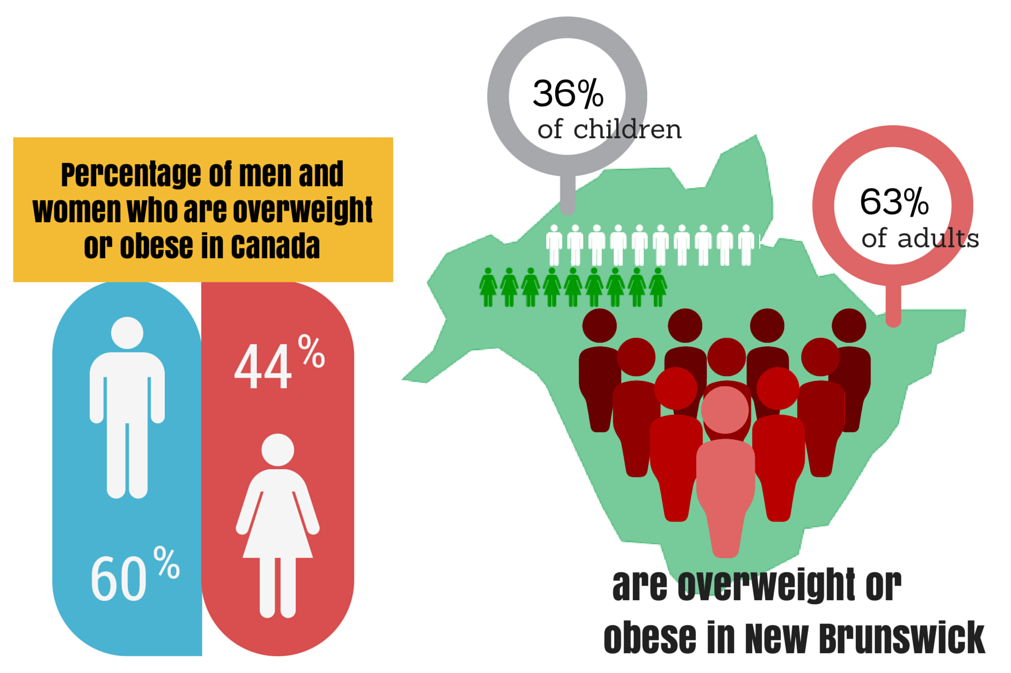
Talking about physical health is difficult without coming across as insensitive, but with 63 per cent of New Brunswick’s adults reporting to be obese or overweight last year, obesity is one of the province’s most expensive problems.
This was the topic of a meeting between the newly-elected president of the New Brunswick Medical Society and the new Health Minister Victor Boudreau Wednesday. It was their first meeting and served to introduce the physician’s lobby group and its goals to the new government.
The medical society pitched legislating schools to offer cooking classes and make physical education mandatory for primary and secondary students, and encouraging fast-food restaurants to offer nutritional information at the counter, among other initiatives, C.E.O. Anthony Knight said.
Last year, the Canadian Institute of Actuarie and the New Brunswick Health Council predicted the total cost of health care in the province would jump almost $2 billion to $4.6 billion between 2009 and 2020. Their study found the average person who is obese costs the system an extra 30 per cent.
It’s not just a tough topic for government, though. With physical health, mental well-being and socioeconomic factors tangled-up in causation and correlation, STU wellness committee chair Lori Orchard said addressing obesity is a challenge for anyone.
“I agree there is a stigma around obesity,” she said. “I think that the way to present anything that has a stigma is to take that negative word out, and to try to relate to the person.”
Orchard said the wellness committee considered running a Biggest Loser-like weight-loss challenge on campus but scrapped the idea, concluding it would do more harm than good. A healthy-cooking seminar is scheduled for January.
The province’s physicians have made many attempts to balance the scales, including giving and taking advice less intrusively through social media channels, and prescribing exercise to patients with a real prescription note, rather than just suggesting it.
Knight said about 50,000 of those prescriptions were given in 18 months.
“I think (overcoming) obesity comes down to individuals, and wanting to try and find ways to make a difference,” he said. “It doesn’t have to be a huge leap in change. It can be literally one step at a time.”
STU students’ union vice-president of student life Rebecca Ferris agrees. She said like mental illness, the reasons for a person’s physical condition are complicated.
“People do have to help themselves, but in order to do that, you need to have an open discussion,” she said. “I don’t know why people shame others for being obese. I don’t think personally attacking anyone helps.”
While STUSU doesn’t have any programs or activities planned to tackle the issues of fitness and nutrition, it has, like many other students’ unions, campaigned to de-stigmatize mental illness.
Inside UNB’s Student Union Building, the “It’s Not About Food” initiative is open to STU students and features a Friday drop-in clinic with varying workshops and freebies like massage therapy, meditation and healthy eating. Last week, Booster Juice was represented as students were taught to make a healthy smoothie.
Knight agreed one can never know the factors behind why a person is fat, but poverty is often one. Research consistently concludes healthy diets cost hundreds to thousands of dollars more per year than eating unhealthily.
“We recognize that socioeconomic factors play a role in peoples’ health outcomes, and we’re conscientious of that, but certain things doctors can do in their offices to make an impact today are really important to us, too.”
With so much talk of obesity leading to expensive medical problems, it is often overlooked that mental illness, medications such as insulin, and medical issues like Cushing syndrome that can cause glands to work improperly and hormones to fall out of balance, can all contribute to obesity.
Ferris said she must be especially careful because diabetes runs in her family. Her grandmother once needed a surgery related to the disease.
“They flat-out told her ‘You need to lose weight before you can do that (surgery),’” Ferris said. “Some people might be insulted. She wasn’t at all. It is a real health issue, and it can be a little bit scary… but I think when it’s a doctor prescribing it it’s a little easier to handle mentally.”
Ferris said weight concerns are not too small of a problem to seek attention for. A physician can find the underlying causes and help to correct them.
Orchard, who is a human resources officer at STU, said she tries to show people facts and let them make decisions themselves.
“I think the fine line we take would be to provide education on living healthy. That’s a good term – not ‘eating nutritiously’, not ‘working out,’ just ‘living healthy’: Taking care of your body. Taking care of your mind.”
